BSDS: ثنائي القطب 1 مقابل ثنائي القطب 2 - شرح الفروق الرئيسية
قد يبدو التنقل في عالم الصحة النفسية وكأنك تحاول قراءة خريطة بلغة أجنبية. تُستخدم مصطلحات مثل اضطراب ثنائي القطب غالبًا، ولكن الفروق الدقيقة بين أشكاله المختلفة يمكن أن تكون مربكة. يتساءل الكثير من الناس، ما الفرق بين ثنائي القطب 1 و 2؟ إن فهم هذا التمييز ليس أكاديميًا فقط؛ بل هو خطوة حاسمة نحو الوضوح، والتواصل الفعال مع مقدمي الرعاية الصحية، وإيجاد المسار الصحيح للمضي قدمًا. يعد مقياس التشخيص الطيفي للاضطراب ثنائي القطب (BSDS) أداة مصممة للمساعدة في تحقيق بعض من هذا الوضوح.
إذا شعرت يومًا بأن مزاجك يتأرجح بين ارتفاعات وانخفاضات شديدة، فأنت لست وحدك. يمكن لهذه التجارب أن تكون مربكة، والحصول على فهم مبدئي لتحديد موقع أعراضك على طيف اضطراب ثنائي القطب هو خطوة أولى قوية. للبدء في استكشاف تجاربك الخاصة بطريقة خاصة وآمنة، يمكنك الحصول على توضيح مع تقييمنا الذاتي للـ BSDS اليوم.
فهم أنواع اضطراب ثنائي القطب
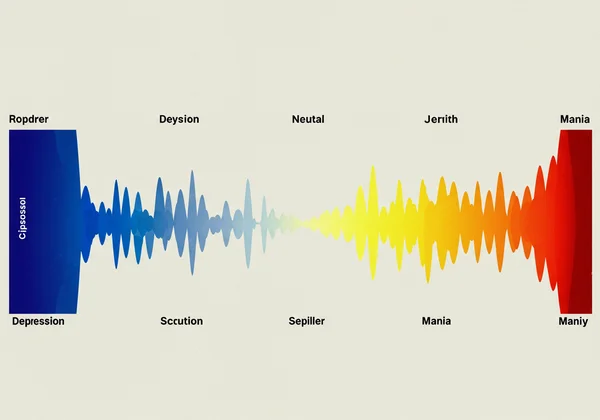
قبل الغوص في تفاصيل اضطراب ثنائي القطب الأول والثاني، من المفيد استيعاب المفهوم الأوسع الذي ينتميان إليه. اضطراب ثنائي القطب ليس حالة واحدة تناسب الجميع. بدلًا من ذلك، فهو موجود على طيف مستمر، ولهذا السبب يشير الخبراء غالبًا إلى طيف اضطراب ثنائي القطب. يعترف هذا المنظور بالنطاق الواسع للأعراض والشدة التي يمكن للأفراد تجربتها.
لفهم الأنواع المختلفة، ركز على وجود وشدة نوبات مزاج معينة، وبشكل أساسي الهوس، والهوس الخفيف، والاكتئاب. الاعتراف بهذه الاختلافات أمر حيوي، حيث يمكنها أن تؤثر بشكل كبير على حياة الفرد وتتطلب استراتيجيات إدارة وعلاج مختلفة.
ما الذي يحدد طيف اضطراب ثنائي القطب؟
طيف اضطراب ثنائي القطب هو مفهوم يشمل ليس فقط ثنائي القطب الأول والثاني، بل أيضًا اضطرابات المزاج ذات الصلة التي لا تتناسب تمامًا مع هذه الفئات. يدرك هذا المفهوم أن تغيرات المزاج يمكن أن تختلف بشكل كبير من شخص لآخر. قد يعاني البعض من نوبات شديدة وموهنة، بينما قد يعاني آخرون من تغيرات أكثر دقة، ولكنها لا تزال معطلة، في المزاج والطاقة. تساعد أداة فحص مثل استبيان اضطراب المزاج في تحديد الأنماط التي قد تشير إلى موقع محتمل على هذا الطيف، مما يوفر نقطة انطلاق قيمة للمحادثة مع متخصص.
لماذا التمييز بين الأنواع؟
يعد التمييز بين اضطراب ثنائي القطب الأول والثاني أمرًا بالغ الأهمية لعدة أسباب. أولًا، يمكن أن تختلف أساليب العلاج. بينما غالبًا ما يشمل كلاهما مثبتات المزاج، فإن الأدوية المحددة والاستراتيجيات العلاجية قد تكون مصممة خصيصًا لنوع وشدة نوبات المزاج. ثانيًا، يختلف التأثير على حياة الشخص. غالبًا ما تؤدي نوبة الهوس الكاملة، التي تميز اضطراب ثنائي القطب الأول، إلى ضعف وظيفي أكثر حدة من الهوس الخفيف الذي يُرى في اضطراب ثنائي القطب الثاني. يساعد فهم تجاربك المحددة في تطوير آليات التأقلم وأنظمة الدعم التي تناسبك.
ثنائي القطب 1 مقابل ثنائي القطب 2: الفروق الأساسية
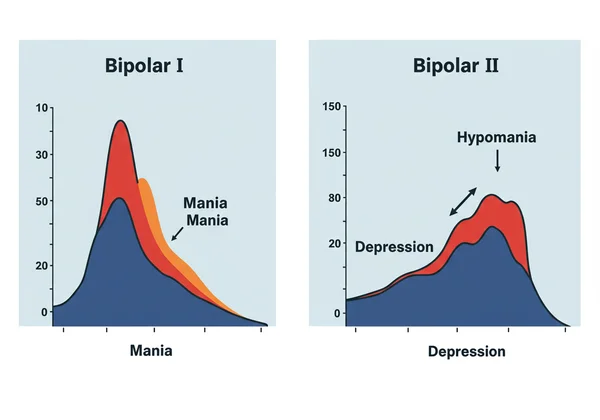
يقع الاختلاف الأساسي بين اضطراب ثنائي القطب الأول والثاني في شدة نوبات المزاج المرتفع. بينما يشمل كلاهما تقلبات مزاجية كبيرة تتضمن انخفاضات اكتئابية، فإن طبيعة "الارتفاعات" هي التي تفصل بينهما. هذا التمييز هو حجر الزاوية في التشخيص.
إذا كنت تحاول فهم أنماط مزاجك الخاصة، فإن النهج المنظم يمكن أن يكون مفيدًا للغاية. يمكنك بدء تقييمك الذاتي للـ BSDS للحصول على رؤى أولية حول أعراضك.
فك رموز اضطراب ثنائي القطب الأول
يُعرّف اضطراب ثنائي القطب الأول بوجود نوبة هوس واحدة على الأقل. هذا هو المعيار التشخيصي الرئيسي. نوبة الهوس هي فترة من المزاج المرتفع، أو المتسع، أو المتهيج بشكل غير طبيعي ومستمر وزيادة في الطاقة، تستمر لمدة أسبوع واحد على الأقل وتوجد معظم اليوم، تقريبًا كل يوم.
تكون الأعراض أثناء نوبة الهوس شديدة بما يكفي للتسبب في ضعف كبير في الأداء الاجتماعي أو المهني أو غيره من مجالات الحياة الهامة. في بعض الحالات، يكون دخول المستشفى ضروريًا لضمان السلامة، أو قد تشمل النوبة سمات ذهانية مثل الهلوسات أو الأوهام. بينما يعاني الأفراد المصابون بثنائي القطب الأول أيضًا من نوبات اكتئاب، فإن وجود نوبة هوس كاملة هو ما يحدد التشخيص.
استكشاف اضطراب ثنائي القطب الثاني
يتميز اضطراب ثنائي القطب الثاني بنمط من نوبات الاكتئاب ونوبات الهوس الخفيف، ولكن ليس نوبات الهوس الكاملة التي تُرى في اضطراب ثنائي القطب الأول. نوبة الهوس الخفيف لها أعراض مشابهة لنوبة الهوس ولكنها أقل شدة. يجب أن تستمر لمدة أربعة أيام متتالية على الأقل وأن يلاحظها الآخرون، ولكنها لا تسبب ضعفًا كبيرًا في الحياة اليومية أو تتطلب دخول المستشفى.
غالبًا ما يطلب الأشخاص المصابون باضطراب ثنائي القطب الثاني المساعدة خلال نوبات الاكتئاب لديهم، حيث قد تبدو فترات الهوس الخفيف منتجة أو حتى ممتعة. قد لا يتعرفون على مزاجهم المرتفع كجزء من نمط أكبر. لهذا السبب، يمكن أن يكون فحص BSDS شاملًا أمرًا مفيدًا للغاية، لأنه يطرح أسئلة تساعد في ربط هذه الحالات التي تبدو منفصلة.
التنقل في نوبات الهوس والهوس الخفيف
يعد فهم التجربة الذاتية للهوس مقابل الهوس الخفيف أمرًا أساسيًا للتفريق بين اضطراب ثنائي القطب الأول والثاني. بينما يتشاركون في أعراض مماثلة - مثل زيادة الثرثرة، وتسارع الأفكار، وانخفاض الحاجة للنوم - فإن شدتها وتأثيرها عالمين مختلفين.
الهوس: السمة المميزة لاضطراب ثنائي القطب الأول
نوبة الهوس هي انحراف كبير عن شخصية الفرد المعتادة. إنها ليست مجرد الشعور بالسعادة أو الحصول على الكثير من الطاقة؛ إنها حالة شديدة يمكن أن تؤدي إلى سلوكيات اندفاعية ومحفوفة بالمخاطر، مثل الإنفاق المتهور، أو القمار، أو اللقاءات الجنسية غير الآمنة. غالبًا ما يكون حكم الفرد ضعيفًا.
مستوى الطاقة مرتفع جدًا لدرجة أنه يمكن أن يكون طاغيًا، والمزاج، على الرغم من كونه مبهجًا في بعض الأحيان، يمكن أن يتحول بسرعة إلى تهيج وانفعال شديد. هذه الشدة هي السمة المميزة لاضطراب ثنائي القطب الأول وسبب رئيسي لأهمية التشخيص الواضح للسلامة والاستقرار.
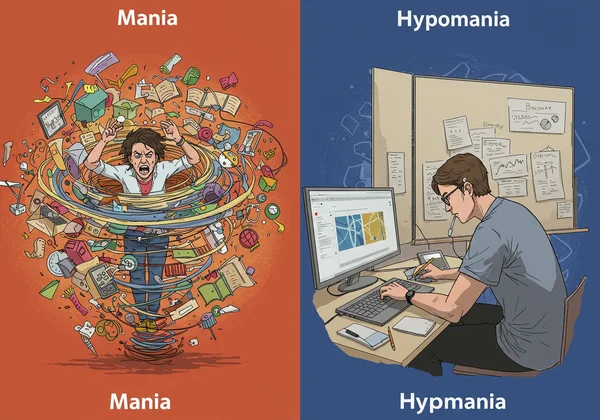
الهوس الخفيف: التجربة غير المعلنة لاضطراب ثنائي القطب الثاني
الهوس الخفيف هو نسخة أقل شدة من الهوس. خلال نوبة الهوس الخفيف، قد يشعر الشخص بزيادة غير عادية في النشاط والإبداع والإنتاجية. قد ينامون أقل ولكنهم لا يشعرون بالتعب. بالنسبة للمراقب الخارجي، قد يبدو أنهم في مزاج جيد بشكل خاص أو "في قمة عطائهم".
ومع ذلك، بينما لا يسبب الهوس الخفيف اضطرابًا كبيرًا في الحياة كما يفعل الهوس، فإنه لا يزال انحرافًا عن حالة الشخص الطبيعية وهو جزء من الطبيعة الدورية لاضطراب ثنائي القطب الثاني. غالبًا ما يتبعه انهيار إلى نوبة اكتئاب كبرى، والتي يمكن أن تكون شديدة وطويلة الأمد. التعرف على الهوس الخفيف هو جزء حاسم لفهم الصورة الكاملة لاضطراب ثنائي القطب الثاني.
طيف اضطراب ثنائي القطب وكيف يقدم BSDS رؤى
مفهوم الطيف تمكيني لأنه يتجاوز التسميات الصارمة. إنه يعترف بأن تجربة كل شخص فريدة. وهنا يبرز دور مقياس التشخيص الطيفي للاضطراب ثنائي القطب (BSDS) كمورد قيم. يساعد في التقاط الفروق الدقيقة لتجارب المزاج التي قد تشير إلى حالة ضمن طيف اضطراب ثنائي القطب.
ما وراء التسميات: الاعتراف بالطيف الأوسع
يساعد التفكير من حيث طيف على تقليل الوصمة وتشجيع نظرة شمولية للصحة النفسية. يسمح بالاعتراف بالأعراض التي قد لا تلبي المعايير الصارمة لاضطراب ثنائي القطب الأول أو الثاني، ولكنها لا تزال تسبب ضيقًا كبيرًا. هذه النظرة الدقيقة ضرورية للفهم الذاتي ولإجراء محادثات مثمرة مع المتخصصين في الرعاية الصحية. غالبًا ما تبدأ رحلة فهم صحتك النفسية بخطوة واحدة، مثل إجراء فحص BSDS مجاني.
كيف يسلط BSDS الضوء على الطيف بالنسبة لك
BSDS هو استبيان تقييم ذاتي مُدققة وذات صلاحية مثبتة علميًا يساعد في تحديد الأعراض والتجارب الرئيسية المرتبطة بطيف اضطراب ثنائي القطب. يطرح أسئلة حول تاريخك الشخصي مع تقلبات المزاج، وتغيرات الطاقة، وأنماط التفكير بطريقة منظمة. التقييم الذاتي للـ BSDS ليس أداة تشخيصية، ولكنه يوفر درجة شخصية يمكن أن تسلط الضوء على مجالات القلق المحتملة.
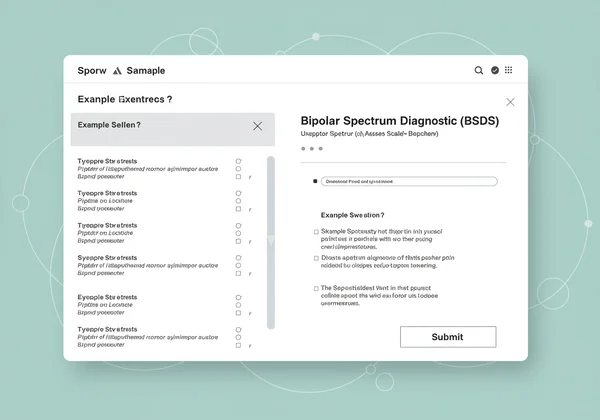
من خلال إكمال التقييم على منصة مثل أداتنا عبر الإنترنت للـ BSDS، تحصل على تقرير سري يمكن أن يكون بمثابة جسر لاستشارة مهنية. يمنحك اللغة وملخصًا منظمًا لتجاربك لمشاركتها مع طبيب أو معالج، مما يجعل تلك المحادثة الأولى أسهل بكثير.
تمكين نفسك: الخطوات التالية لفهم أعراض اضطراب ثنائي القطب
يعد فهم الاختلافات بين اضطراب ثنائي القطب الأول والثاني أمرًا حيويًا. هذا التمييز، الذي يركز على الهوس مقابل الهوس الخفيف، يؤثر بشكل كبير على حياة الفرد وعلاجه وإدارته. إدراك أن هذه الحالات موجودة على طيف يمكن أن يساعدك في فهم تحولات مزاجك الفريدة.
المعرفة قوة، والخطوة الأولى نحو إدارة صحتك النفسية هي فهمها. إذا كان هذا المقال قد لامس شيئًا بداخلك، ففكر في اتخاذ الخطوة التالية. يمكن لأداة مثل مقياس التشخيص الطيفي للاضطراب ثنائي القطب أن توفر رؤى قيمة وخاصة.
هل أنت مستعد للحصول على صورة أوضح؟ أجرِ اختبار BSDS الخاص بنا اليوم. إنه مجاني وسري وخطوة شجاعة في رحلتك نحو العافية.
أسئلة متكررة حول أنواع اضطراب ثنائي القطب و BSDS
ما مدى دقة اختبار BSDS في تحديد أعراض طيف اضطراب ثنائي القطب؟
مقياس التشخيص الطيفي للاضطراب ثنائي القطب (BSDS) هو أداة فحص مُدققة وذات صلاحية مثبتة مع حساسية مثبتة للكشف عن أعراض اضطراب ثنائي القطب. ومع ذلك، فهو ليس اختبارًا تشخيصيًا. الغرض منه هو تحديد الأفراد الذين قد يستفيدون من تقييم سريري كامل. الدقة العالية في سياق الفحص تعني أنه يشير بفعالية إلى المشكلات المحتملة للمراجعة المهنية.
هل يعد BSDS تشخيصًا نهائيًا لاضطراب ثنائي القطب؟
لا، على الإطلاق. BSDS هو أداة فحص، وليست أداة تشخيص. لا يمكن إجراء تشخيص نهائي لاضطراب ثنائي القطب إلا بواسطة متخصص رعاية صحية مؤهل، مثل طبيب نفسي أو أخصائي نفسي، بعد تقييم شامل يتضمن مقابلة سريرية ومراجعة لتاريخك الطبي الشخصي والعائلي. نتائج التقييم السري للـ BSDS الخاص بنا هي نقطة انطلاق لتلك المحادثة.
ما هي العلامات العامة لاضطراب ثنائي القطب التي يجب الانتباه إليها؟
تشمل العلامات العامة تقلبات مزاجية دراماتيكية وغير متوقعة. يمكن أن تتراوح هذه من فترات طاقة مكثفة، أو ابتهاج، أو تهيج (الهوس أو الهوس الخفيف) إلى فترات حزن عميق، أو يأس، أو طاقة منخفضة (الاكتئاب). تشمل العلامات الأخرى تغيرات في أنماط النوم، ومستويات النشاط، والأفكار، والسلوك التي تمثل انحرافًا واضحًا عن ذاتك الطبيعية.
هل يمكن لاختبار التمييز بين الاكتئاب ثنائي القطب والاكتئاب أحادي القطب؟
هذا تحدٍ رئيسي في مجال الصحة النفسية. بينما يمكن أن تبدو نوبات الاكتئاب نفسها متطابقة، فإن أداة فحص مثل BSDS تساعد عن طريق طرح أسئلة محددة حول التجارب السابقة أو الحالية للمزاج المرتفع (الهوس أو الهوس الخفيف). وجود هذه "الارتفاعات" هو العامل الأساسي الذي يميز الاكتئاب ثنائي القطب عن الاكتئاب أحادي القطب، وتم تصميم BSDS لتحديد تلك التجارب.