Bipolar Spectrum Disorder: Symptoms, Types & BSDS Explained
Navigating the world of mental health can feel overwhelming. Terms are complex, symptoms overlap, and it's easy to feel lost. If you've found yourself questioning intense mood swings—your own or a loved one's—you're not alone. The journey to understanding often begins with a single question: What are the signs of bipolar disorder? This guide is designed to provide clarity, breaking down Bipolar Spectrum Disorder into understandable parts and introducing a valuable tool to help you take a proactive first step.
Bipolar disorder is more than just feeling happy one day and sad the next; it's a serious medical condition characterized by significant shifts in mood, energy, and activity levels. Understanding its nuances is the first step toward empowerment. On our platform, we believe that accessible, science-backed information is crucial for this journey. We offer a validated screening tool that can help you gain some clarity on your experiences.
What is Bipolar Spectrum Disorder (BSD)?
Bipolar Spectrum Disorder (BSD) is a category of mental health conditions defined by extreme mood episodes that range from manic highs (mania or hypomania) to depressive lows. Rather than viewing bipolar disorder as a single, rigid diagnosis, the "spectrum" concept acknowledges that the condition manifests in many different ways, with varying intensity and frequency of episodes.
This modern understanding helps capture the experiences of many individuals who may not fit neatly into the classic definitions but still face significant challenges from mood instability. It allows for a more personalized and accurate approach to both assessment and treatment.
Beyond "Manic Depression": Understanding the Spectrum
For many years, the term "Manic Depression" was used to describe this condition. While it captured the core duality of mania and depression, it oversimplified the experience. The term "Bipolar Spectrum" is now favored by clinicians because it better represents the wide range of symptoms and severities. Think of it less like a switch that's either on or off, and more like a dial that can be turned to various degrees, encompassing everything from severe manic episodes to milder, but still disruptive, mood fluctuations.

How Common is Bipolar Disorder? Prevalence & Demographics
Bipolar Spectrum Disorder is more common than many realize. The National Institute of Mental Health (NIMH) estimates that 2.8% of U.S. adults experience it annually, affecting men and women nearly equally. While the average age of onset is the late teens or early 20s, it can appear at any age.
Recognizing the Key Signs & Symptoms of Bipolar Disorder
Identifying the signs of bipolar disorder involves looking for distinct periods of unusually intense emotion and changes in behavior, known as mood episodes. These are distinctly different from a person's usual self.
The Peaks: Mania & Hypomania
Mania and hypomania represent the "highs" of the bipolar spectrum, differing primarily in severity. Mania causes significant impairment and may require hospitalization, whereas hypomania is less severe.
Symptoms can include:
- An abnormally upbeat, jumpy, or wired feeling
- Increased energy, activity, and agitation
- An exaggerated sense of well-being and self-confidence (euphoria)
- Decreased need for sleep
- Unusual talkativeness and racing thoughts
- Distractibility
- Poor decision-making, such as engaging in risky behavior
The Valleys: Bipolar Depressive Episodes
The "lows" are characterized by debilitating bipolar depressive episodes, which often last longer than manic or hypomanic periods.
Symptoms can include:
-
Feeling sad, empty, hopeless, or worthless
-
Marked loss of interest or pleasure in all, or almost all, activities
-
Significant weight loss or gain, or a decrease or increase in appetite
-
Insomnia or sleeping too much
-
Restlessness or slowed behavior
-
Fatigue or loss of energy
-
Difficulty concentrating, remembering, or making decisions
-
Thinking about, planning, or attempting suicide

Mixed Features and Rapid Cycling: When Symptoms Overlap
The lines between mania and depression can blur, leading to "mixed features" episodes with simultaneous manic and depressive symptoms (e.g., feeling energized yet hopeless). Another pattern, "rapid cycling," involves four or more mood episodes within a year. These complex presentations underscore the need for a professional assessment.
Understanding the Different Types of Bipolar Disorder
The bipolar spectrum is officially categorized into several types to help clinicians create the most effective treatment plans.
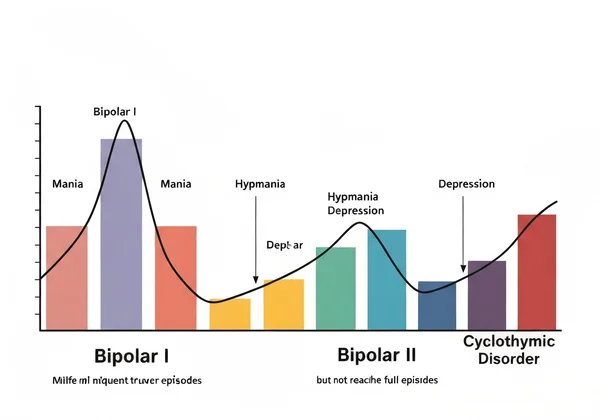
Bipolar I, Bipolar II, and Cyclothymic Disorder
-
Bipolar I Disorder: Defined by at least one manic episode. This manic episode may be preceded or followed by hypomanic or major depressive episodes. The mania is severe enough to cause significant disruption to work, school, or relationships.
-
Bipolar II Disorder: Defined by at least one hypomanic episode and at least one major depressive episode. Individuals with Bipolar II have never had a full manic episode. The periods of depression are often longer and more impairing than the hypomania.
-
Cyclothymic Disorder: Characterized by at least two years (one year in children and adolescents) of many periods with hypomanic symptoms and periods with depressive symptoms that do not meet the full criteria for a major depressive episode.
Other Specified and Unspecified Bipolar and Related Disorders
This category applies to individuals whose symptoms cause significant distress but don't perfectly match the criteria for the other types. This ensures that everyone who struggles with bipolar-like symptoms can receive a diagnosis and get help, reinforcing the importance of the spectrum approach.
Why a Professional Diagnosis for Bipolar Disorder is Crucial
While self-assessment is a helpful first step, it cannot replace a clinical evaluation. Only a qualified healthcare professional, such as a psychiatrist or psychologist, can provide an accurate diagnosis.
The Risks of Misdiagnosis and Delayed Treatment
Bipolar disorder is often misdiagnosed as unipolar depression or anxiety, leading to ineffective or even harmful treatments. For instance, certain antidepressants can trigger mania if prescribed without a mood stabilizer. Delayed treatment can worsen outcomes, making a thorough, accurate assessment critical to start the conversation with a professional.
Benefits of Early Intervention and Tailored Treatment Plans
An accurate diagnosis is a turning point, enabling effective, tailored treatment plans that may include medication, psychotherapy, and lifestyle strategies. Early intervention significantly improves long-term outcomes by helping individuals manage symptoms, reduce episode frequency, and lead fulfilling lives.

The Role of Screening Tools: Introducing the BSDS
If you suspect you're on the bipolar spectrum, a validated screening tool is an excellent starting point. It offers a structured way to review your experiences, providing valuable information to share with a doctor.
What the Bipolar Spectrum Diagnostic Scale (BSDS) Assesses
The Bipolar Spectrum Diagnostic Scale (BSDS) is a scientifically validated self-assessment tool designed to help identify symptoms associated with the bipolar spectrum. It was developed by Dr. Ronald Pies and is widely respected in the clinical community. The BSDS focuses on mood shifts, energy levels, and behavioral patterns that characterize the "highs" of the spectrum, which are often the key differentiators from other mood disorders. It can provide an initial indication of whether your symptoms warrant further professional evaluation. You can take the BSDS screening right here on our platform.
BSDS vs. Other Screening Tools: A Brief Comparison
While other tools like the Mood Disorder Questionnaire (MDQ) exist, the BSDS is unique for its narrative-based format. It encourages users to reflect on their experiences in the context of their "best and most energetic self," which helps capture the subtle changes of hypomania and provides a nuanced score reflecting the spectrum nature of the condition.
What Your BSDS Screening Results Mean (and What They Don't)
After completing the assessment, you will receive a score. It’s vital to understand what this score represents. A higher score suggests that your experiences align with those commonly seen in Bipolar Spectrum Disorder and indicates that a follow-up conversation with a healthcare professional is strongly recommended.
However, your score is not a diagnosis. It is a data point—a piece of evidence to help you and your doctor explore your mental health more deeply. Many factors contribute to a formal diagnosis, which can only be made after a comprehensive clinical interview.
Taking Your Next Step: Towards Clarity and Action
Your journey towards understanding mood patterns begins with taking an informed step. The BSDS screening tool empowers you with objective information, helping you organize your thoughts and prepare for a productive conversation with a healthcare provider. A screening tool like the BSDS can bridge the gap between wondering and knowing what to do next.
Ready to take the first step towards understanding your mood patterns? Start Your BSDS Assessment now. It's free, confidential, and based on a scientifically validated scale.
Frequently Asked Questions About Bipolar Spectrum Disorder & BSDS
What is the Bipolar Spectrum Diagnostic Scale (BSDS)?
The Bipolar Spectrum Diagnostic Scale (BSDS) is a validated self-report questionnaire that helps identify symptoms associated with Bipolar Spectrum Disorder. It is a screening tool, not a diagnostic test, meant to facilitate a conversation with a healthcare professional.
What is the diagnostic scale for bipolar disorder?
No single scale can definitively diagnose bipolar disorder. A diagnosis requires a comprehensive clinical evaluation by a qualified professional, including a detailed interview. Screening tools like the BSDS are used to determine if a full evaluation is recommended.
What are the signs of bipolar disorder?
The primary signs are distinct mood episodes, including manic or hypomanic "highs" (e.g., elevated energy, racing thoughts, decreased need for sleep) and depressive "lows" (e.g., profound sadness, loss of interest, fatigue). The intensity and pattern of these episodes vary across the bipolar spectrum.
Is the BSDS a definitive diagnosis for bipolar disorder?
No, absolutely not. The BSDS is a highly reliable screening tool, but it cannot provide a diagnosis. Think of it like taking your temperature when you feel sick—a high reading suggests you should see a doctor, but it doesn't tell you what illness you have. A diagnosis can only be made by a qualified mental health professional after a thorough assessment. We encourage you to get your initial screening results and share them with a provider.
What is the difference between Bipolar I and Bipolar II?
The main difference lies in the severity of the "high" episodes. Bipolar I is defined by the presence of at least one full manic episode, which is a period of severe mood elevation that significantly impairs functioning. Bipolar II is characterized by less severe highs, known as hypomania, along with at least one major depressive episode.